
What are Tailored Plans?
Tailored Plans are a new type of Medicaid managed care plan administered by private companies for beneficiaries with more complex health needs. Tailored Plans are specifically for people with intellectual/developmental disabilities, mental health disorders, substance use disorders, or traumatic brain injuries.
Tailored Plans will also serve people on the NC Innovations Waiver or Traumatic Brain Injury (TBI) Waiver. People will not lose their spots on the waitlist.
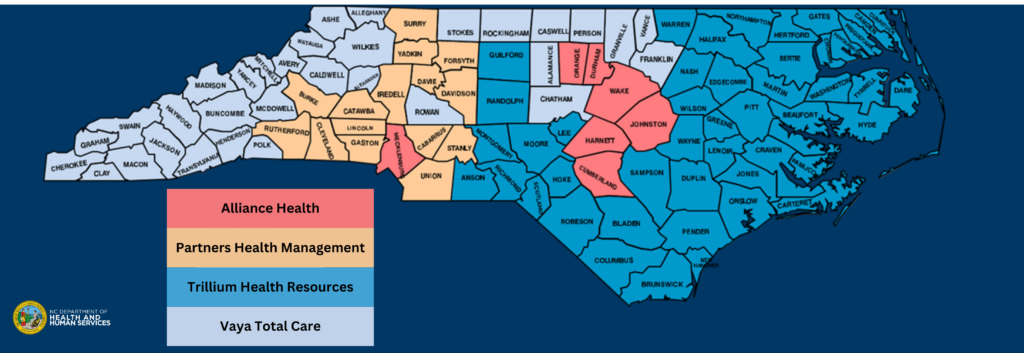
Tailored Plans are run by the following four companies known as Local Management Entities (LME): Alliance Health, Trillium Health Resources, Partners Health Management, and Vaya Total Care. The LMEs will cover a wide range of services including behavioral health, physical health, and prescription needs for Tailored Plan beneficiaries.
Alliance Health is the only Tailored Plan that currently offers TBI Waiver services. To learn more about Tailored Plans, click here.
These plans go live on July 1, 2024.
How do I know which Tailored Plan I am in?
You should receive a letter from either Alliance Health, Trillium Health Resources, Partners Health Management, or Vaya Total Care. For the vast majority of Tailored Plan beneficiaries, you will be assigned to a plan depending on the county you live in. However, for some people who live in group homes or facilities, their Tailored Plan will be based off the county they lived in prior to the facility. The map below shows the coverage area for each Tailored Plan according to county. You cannot switch to a different Tailored Plan.
How are Tailored Plans different from what the LMEs offer now?
Currently, LME/MCOs only manage behavioral health services. Once Tailored Plans go live, they will manage all Medicaid services for beneficiaries including physical health services, pharmacy, and more.
How do Tailored Plans work?
Unlike with Medicaid Standard Plans, which are mostly offered statewide and allow beneficiaries to choose their Standard Plan, Tailored Plan beneficiaries will be assigned to a Tailored Plan depending on the county they live in without the option to switch to a different Tailored Plan.
Each Tailored Plan has its own network of providers.
How do I know if my provider is in my Tailored Plan’s network?
There are two ways to check if your provider is in your Tailored Plan network.
- Call your Tailored Plan directly.
- Alliance Health, 1-800-510-9132, TTY: 711 or 1-800-735-2962
- Partners Health Management, 1-888-235-4673, TTY/English: 1-800-735-2962, TTY/Spanish: 1-888-825-6570
- Trillium Health Resources, 1-877-685-2415, TTY: 711
- Vaya Total Care, 1-800-962-9003, TTY: 711
- Try looking up your provider in the Medicaid provider directory by going to ncmedicaidplans.gov/en/find-provider. Please note that the directory may not be completely up to date.
Can I still see my provider or specialist even if they aren’t in my Tailored Plan Network?
Even if your provider or specialist isn’t in your Tailored Plan network, hopefully you can continue getting services from them until January 31, 2025. If you don’t believe your specialist or provider is in your Tailored Plan network, call your Tailored Plan to request them to reach out to the provider you need.
What do Tailored Plans offer?
Tailored Plans offer the same services as Standard Plans plus additional support services for people with SUD, TBI, I/DD, or a mental health disorder. Examples of these additional support services are intensive in-home care, psychosocial rehabilitation, residential treatment facility, etc. For more information on Tailored Plan services, please go here.
Additionally, the services listed below are only available with a Tailored Plan.
- Innovations Waiver services
- Intermediate Care Facility for individuals with Intellectual Disabilities (ICF-IID) services
- State-Funded (non-Medicaid) services
- TBI Waiver services
- Transitions to Community Living (TCL) program services
What if I don’t want to be in a Tailored Plan?
Call the N.C. Medicaid Ombudsman at 877-201-3750 for assistance to disenroll from a Tailored Plan into a Standard Plan, Medicaid Direct, or to simply get more information. The Medicaid Ombudsman has live customer service agents from 8 am to 5 pm Monday through Friday. The Medicaid Ombudsman operates with a “no-wrong door” approach, so they will make sure to either directly help you with your question or refer you to someone who can.
For more information on Tailored Plans, visit the NC Medicaid Ombudsman website or the NC DHHS website.
 Justice Circle
Justice Circle